Third Sun
February 06, 2018
All Care Health Center
Published in
General
Tagged under
December 11, 2016
Five Things You Need to Know about Getting Health Coverage in Iowa
Enrolling in health care coverage can be confusing, so we’ve put together a list of five help things you should know before you enroll.
- The Marketplace is open for business. The fourth open enrollment period for the Health Insurance Marketplace is underway for those looking to renew their current runs from November 1, 2016 through January 31, 2017. Consumers can enroll in Medicaid at any time throughout the year.
- Financial assistance may be available. While insurance premiums have increased for some consumers, most will not see a higher cost due to the increase in the subsidies available to help individuals afford the cost of their coverage. If purchasing coverage through the Marketplace, consumers could be eligible for tax credits or subsidies to help offset the cost.
Need coverage on January 1? In order for a person to have coverage effective starting January 1, 2017, individuals must enroll in a plan by December 15. - We’re here to help! In-person assistance is available free of charge at community health centers located across the state of Iowa. A Certified Application Counselor (CAC) can assist consumers with enrolling in coverage and determining eligibility for both Marketplace plans and Medicaid. Click here to locate a health center near you.
- Concerned about losing your health coverage? While there is uncertainty about the future of the Affordable Care Act and plans offered through the Health Insurance Marketplace, it is still important to make sure you have health coverage for 2017.
For more information about the Health Insurance Marketplace, visit healthcare.gov. Individuals can enroll in Marketplace coverage at healthcare.gov or by calling 1 (800) 318-2596 (TTY: 1 855 889-4325).
Published in
Iowa PCA Blog
Tagged under
February 27, 2017
Vital Performance Improvement – Blood Pressure Competency Training
It’s something everyone has experienced during a visit to a clinic. We all know it’s going to happen so we roll up our sleeve, mat down our sweater, or take off our jacket after our temperature and weight has been taken. Blood pressure is one of the vital signs yet such a simple and routine process in health care can be complex.
Even the smallest increases in blood pressure above normal reduces life expectancy and have a significant impact on the health of patients. In people with hypertension and elevated blood pressure, when blood pressure is lowered there is less vascular damage to organs (kidneys, heart, eyes, brain) and the treatment of high blood pressure lowers risk of cardiovascular disease and death. While it is important to note that we can’t eliminate the risks associated with having high blood pressure entirely by driving blood pressure back down to normal, we can lower the risk of heart attack, stroke, and death by controlling blood pressure.
Setting Standard, Together
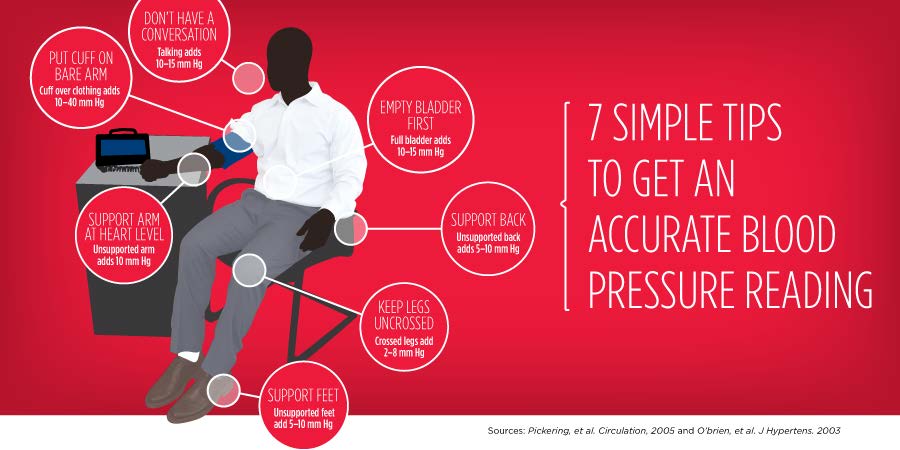
Eleven of the health centers in Iowa have set a standard for improving blood pressure control rates and we had to start at the ground level with blood pressure competencies. The Iowa PCA performance improvement team began by working with each health center to assess each clinics’ ability to take accurate blood pressure. Were the exam rooms set up so that an accurate reading could occur? Had the blood pressure equipment been calibrated? Was the cuff placed over clothing, was the cuff the right size, was the patient talking, had they rested for five minutes before the measures was taken, was their back, arm, and feet supported, were their legs crossed and did they have a full bladder? A no response to any of these questions can account for inaccurate blood pressure measurement.
We then worked with a subcommittee of health center staff to develop a patient engagement and education toolkit and developed a consistent approach to training and retraining of staff on at least an annual basis. And, part of this work involved how to engage the patients in helping to ensure they were in the right position for the measurement to occur. Many of the health centers have now posted the below visual in their exam rooms and it is serving as a meaningful reminder to patients and health center staff.
Once the blood pressure competency training was completed by all the health centers, our Chief Medical Officer, Dr. Michael Piplani who also serves as Chief Medical Officer of Siouxland Community Health Center gassed up his car and completed a “heartfelt” tour to all the health centers to underscore the importance of this work with the health center providers.
More Improvement
Since completing the foundational work of blood pressure competency training, we’ve shifted our focus to the myriad other issues that impact blood pressure control rates. Our recommitment to ensuring blood pressures are being taken appropriately did reduce our control rates, but we are now better-positioned to undertake additional performance improvement work. Our primary focus areas are on recalling patients not in control, assessing our health information technology systems to ensure they are working for staff, beginning to tackle undiagnosed hypertension, integrating clinical pharmacy services, and thinking about how our dental and behavioral health clinics can play a role in identifying patients who need education and support to better control their blood pressure.
Recently, in honor of our recommitment to overall heart health, the Iowa PCA staff wore red during American Heart Month. We commend all the health care and public health professionals across the state that are working to improve the heart health of Iowans. And, three cheers for using less salt, moving more, and for helping to better engage patients in their own care!
Published in
Iowa PCA Blog
Tagged under
March 26, 2017
Calling All Poop Queens and Kings!
Of all the preventive cancer screenings, colorectal cancer has the most stigma, elicits the strongest reactions and fear, and is also the most misunderstood. Therefore, there is no room for bashfulness or modesty when developing plans for patient outreach and recall around colorectal cancer. What is incredible is that colorectal cancer is completely preventable if the health care system, public health, patients, and families all come together to combat this disease.
Through the Iowa PCA’s Performance Improvement Learning Collaborative and our sister company, IowaHealth+, eleven of the health centers agreed to focus on improving their colorectal cancer screening rates. Each health center committed to improve their overall screening rate by 10% (based on their 2015 UDS rate) by 2017 or achieve the 80% target set by the National Colorectal Cancer Roundtable. We found great variability in the screening rates among the health centers and invited four health centers to serve as the initial sites where our performance improvement team would go to work.
Our performance improvement team uses a common methodology for approaching projects in partnership with the health centers. This includes conducting a current state assessment and process maps at each health center followed by the development of a project charter to guide the implementation of the project. After the assessment and process mapping was complete, our team completed several observations onsite at the initial four health centers before identifying gaps and barriers affecting the CRC screening process. We then worked with the health centers through our Clinical Quality and Consumer Advisory Committees to identify recommendations for improvement.
What we found during the observations at four health centers was a mix of cultural and process issues that could either contribute to or restrict the ability of the health centers to affectively reach patients in need of screening. The cultural issues that primarily impact colorectal screening include: 1) the level of empowerment that care team members have to work together to increase screening rates and 2) the comfort level among care team members to talk with patients in an understandable way about the screening (thus the name of this blog post!). The primary process issue that we identified is a lack of effective, consistent, and efficient provider reminder and patient recall systems.
Now that these issues have been identified, we have been working with the four health centers to improve their processes and will spread the same approach to the additional seven health centers over the next three months. Because of the hard work among the health centers and our PI team, we saw a 5.9% increase in our screening rates from 2015 to 2016 based on the Universal Data System measurement, which health centers must report annually to the federal government.
We are thrilled to have support from the Iowa Department of Public Health, the American Cancer Society, and the National Association of Community Health Centers to help us better serve our patients and know that what we have learned from this approach will inform future initiatives to improve other preventive screening rates. There are more poop queens and kings out there than you would think and Iowans will benefit from these committed individuals in the fight to prevent a prevalent disease!
Published in
Iowa PCA Blog
Tagged under
In 2016 it was extremely difficult for a low-income individual living in and around Cedar Rapids, IA to access dental care. According to a report by Linn County Public Health, 45% of low-income adults living in East Central Iowa had not had a dental service in the past year. Additionally, the report highlighted that in 2014 only 51% of Medicaid enrolled children between the ages of 1 – 20 received dental services, including urgent services to treat decay.
After learning of the extraordinary need, Eastern Iowa Health Center decided to tackle the issue of access to care for the underserved population head-on. In 2016, with lead gifts from the Delta Dental of Iowa Foundation and the Hall-Perrine Foundation, EIHC purchased the land and building adjacent to the EIHC primary health care and pediatrics office in Cedar Rapids to create the Eastern Iowa Dental Center. Following months of renovation, the dental center opened to patients in March 2017. In the first three months of operation, EIDC dentists, hygienists and assistants have provided oral healthcare to over 800 patients in 1,539 encounters. The majority of dental center patients live at or below 200% of the Federal Poverty Level and are insured by Medicaid.
The proximity of the dental center to the primary care office strengthens the mission and patient-centered focus of Eastern Iowa Health Center. Patients with an urgent dental need visiting their primary care provider can often be seen by a dentist the same day. Additionally, EIDC is committed to establishing good dental hygiene practices from an early age and works directly with pediatricians to help establish a dental home for children by the age of one. The dental center has created an EIHC healthcare campus that focuses on providing quality care to the most vulnerable and at-risk populations living in East Central Iowa.
Currently EIDC is a six-chair dental office that provides preventive and restorative oral healthcare services, however, the dental center has the space to expand to eight chairs. It is the goal of EIHC to fully outfit EIDC and provide oral surgery services in the near future.
The dental center, which opened in March 2017, is the result of numerous donations and gifts in-kind; the leadership and Board of Directors of EIHC would like to thank the following supporters: Delta Dental of Iowa Foundation, Hall-Perrine Foundation, AEGON-Transamerica Foundation, Diamond V Community Health Free Clinic, Dr. Curtis Livengood, Van Meter Donor-Advised Fund of the Greater Cedar Rapids Community Foundation, DeeAnn McIntyre, McGrath Automotive Group of the Greater Cedar Rapids Community Foundation, Van Meter Donor-Advised Fund of the Greater Cedar Rapids Community Foundation, Henry Schein, Primus Construction and Daybreak Rotary.
Erin Langdon
Eastern Iowa Health Center
Published in
Iowa PCA Blog
Tagged under
River Hills Community Health Center opened their Behavioral Health Program in July of 2011 to meet an increasing need for more mental health services in the community. The need for these services increased after the Ottumwa Regional Health Center was sold to Regional Care, a Nashville, Tennessee based organization, and their Behavioral Health Program was discontinued. Prior to July 2011, five Psychiatrists lived in Ottumwa on a full-time basis, but that number has since decreased to zero. The Psychiatrists who currently practice in Ottumwa do so primarily by Tele-Psychiatry.
I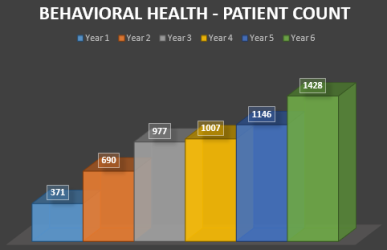 nitially, River Hills Behavioral Health Program started with only two Therapists from Ottumwa Regional Health Center, followed by a third Therapist being hired one month later. After adding a fourth Therapist, River Hills Behavioral Health Program then began Tele-Psychiatry Services in November of 2012. The Program has seen steady growth in client numbers which was bolstered by the hiring of a Board Certified General Psychiatrist in January 2016 who can see all ages. Additionally, a Psychiatric Nurse and a Bi-Lingual Nursing Assistant were also hired.
nitially, River Hills Behavioral Health Program started with only two Therapists from Ottumwa Regional Health Center, followed by a third Therapist being hired one month later. After adding a fourth Therapist, River Hills Behavioral Health Program then began Tele-Psychiatry Services in November of 2012. The Program has seen steady growth in client numbers which was bolstered by the hiring of a Board Certified General Psychiatrist in January 2016 who can see all ages. Additionally, a Psychiatric Nurse and a Bi-Lingual Nursing Assistant were also hired.
Currently River Hills Community Health Center employs nine Therapists in three different Clinic Sites within their eight county service area. These nine Therapists specialize in various styles of Therapy that are effective for all ages. The therapies include: Play Therapy, Art Therapy, Addiction Therapy, Relationship Therapy, Parent Skill Development, Marital Counseling, Anger Management, Conflict Resolution, Depression, and Anxiety Management. Additional Treatment Modalities are also offered depending on the individual needs of the Patient and/or Family.
In late 2016, River Hills Community Health Center continued to expand their Behavioral Health Program by hiring a Doctorate Level Clinical Psychologist who now provides a wide range of Psychological Testing and IQ Testing for both children and adults.
In addition to the Wapello County Behavioral Health Clinic in downtown Ottumwa, there are also now Full-Time Behavioral Health Clinics in both Appanoose County (Centerville) and Keokuk County (Sigourney).
With the recent Wapello County Clinic Expansion Project in Ottumwa, River Hills Community Health Center has nearly doubled the physical size of their Behavioral Health Program which will allow for the hiring of additional Behavioral Health Therapists and Psychiatric Providers in the future.
Although River Hills Behavioral Health Program is not fully integrated physically within all the other departments of the Health Center at this time, patient referrals are continually being made back and forth across the various departments to ensure that comprehensive and holistic care is being provided to all River Hills patients.
Feel free to contact any of River Hills three Behavioral Health Clinic Sites for additional information or to schedule an appointment. The phone numbers are as follows:
Ottumwa (641) 683-5773
Centerville (641) 856-4400
Sigourney (641) 224-8061
Rick Johnson, Brian Simmons, and Steve Lee
River Hills Community Health Center
Published in
Iowa PCA Blog
Tagged under
Imagine your typical day.
You wake up in the morning in a home where you feel safe, eat breakfast, and head to work or school in your car, and have a relatively stress free day.
But what if your day wasn’t that simple? You wake up every morning in a shelter. You aren’t sure where your next meal will come from. You don’t have transportation. What if your child has asthma due to your living conditions, or there aren’t any job openings in your town?
For many people factors such as these, also known as Social Determinants, greatly affect not only their lives but their health. Aspects of everyday life that many take for granted are often barriers for others.
The Iowa Primary Care Association and our community health centers have witnessed over the years how social determinants play a role in the health of our patients. By offering enabling services such as transportation to appointments, connecting patients to social services, and providing interpreters, health centers are at the forefront of addressing these factors to improve the health outcomes of our patients through high quality, cost-effective care.
The Iowa PCA is further expanding our work by capturing the social determinants affecting our patients through a patient survey tool, Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE). Developed in conjunction with the National Association of Community Health Association, the Association of Asian Pacific Community Health Organizations, the Oregon Primary Care Association, and the Institute for Alternative Futures, this national effort aims to help health centers and other providers collect data on their patients’ needs and risks to better target both clinical and non-clinical care. Two health centers in Iowa, Siouxland Community Health Center in Sioux City and Peoples Community Health Clinic in Waterloo, were part of a group of pioneer health centers to test PRAPARE and are currently using the tool. Our staff is also in the process of developing plans to expand to more health centers in Iowa.
The Sioux City Journal published last week a great piece about how Siouxland Community Health Center is using PRAPARE to identify and address the basic needs of their patients.
During the past year, we’ve also partnered with Iowa Legal Aid to test a new Medical-Legal Partnership Model between Community Health Centers and attorneys thanks to a grant from the Telligen Community Initiative. Through this model, Certified Application Counselors at Siouxland Community Health Center and Primary Health Care, Inc. in Des Moines, Ames, and Marshalltown, are able to refer consumers whom may have certain legal needs that affect their health to an attorney employed by Iowa Legal Aid.
As we continue this work, we encourage others in Iowa to join our effort to address the needs of Iowa’s vulnerable populations. In the coming months, we will take a deeper dive into the social determinants of health affecting many low-income Iowans and our work to ensure a healthier future for our patients.
Published in
Iowa PCA Blog
Tagged under
Years ago, the sounds of bowling pins clattering and people laughing echoed through the building. These days, people might hear the tiny cries of a newborn baby or the reassuring voice of a nurse.Since opening nine years ago, Promise Community Health Center has gradually transformed what was once an old bowling alley building into a fully functioning, comprehensive health center in downtown Sioux Center.
The latest evolution of Promise’s facilities is underway.
This spring, the health center completed a 2,200-square-foot interior expansion and remodeling project that filled the remaining available space in the building. Later this summer, a major exterior renovation project will convert the deteriorating, yellow, steel exterior of the building into a much more inviting and modern facade.
Nancy Dykstra, executive director for Promise, said the projects are positive signs of Promise’s growth as it fulfills its mission in the community.
“I believe that Promise Community Health Center will continue to thrive and be a place of service to all who need us now and into the future,” she said. “Everyone is welcome at Promise.” conf Promise Community Health Center staff participate in a training about human trafficking in the new community education/conference room. Promise recently completed an expansion project that filled the remaining available portions of its building.
The interior expansion project included a much larger community education/conference room, two patient rooms and two offices.
The larger meeting room – which is equipped with a refrigerator, microwave, cabinets and a large multimedia screen – provides adequate space for Promise to conduct all-staff meetings and trainings and to host group education sessions, presentations and meetings for community members.
The vision/eye care program will move into one of the exam rooms in the near future, and the second exam room will allow for future growth. The two new offices are occupied by the executive director and chief financial officer.
The project also involved the remodeling and reuse of existing spaces. The former conference room has been divided into four office cubicles – with two allocated to the family planning nurse educator and medical records specialist and two for future staff growth.
A workstation also was freed up for the new nurse health coach in the clinical setting – ensuring that she is accessible and available to the medical team and that the services are integrated. The director of operations and clinic manager now have their own offices instead of sharing one.
 “The expansion project will allow our new services to grow and current services to function more efficiently and effectively,” Dykstra said. “The expansion provides onsite opportunities for staff education, training and an enhanced work environment.”
“The expansion project will allow our new services to grow and current services to function more efficiently and effectively,” Dykstra said. “The expansion provides onsite opportunities for staff education, training and an enhanced work environment.”
Construction for Promise’s exterior renovation project is expected to commence soon.
The exterior walls will be refaced with brick on the bottom third and an EIFS finish on the top two-thirds. A new front doorway and new floor-to-ceiling windows will be installed to bring in additional daylight to Promise’s reception area. The awnings over Promise’s front and back entrances will be replaced with a modern lighted feature. Sidewalks in front of the building will be reconstructed to enhance safety. The roof will be repaired.
The project was made possible due to many donations from individuals and businesses in the community during a $250,000 capital campaign, which was launched during Promise’s eighth annual “An Evening of Promise” Celebration and Fundraiser on Nov. 3. “Improving the exterior of the building for Promise is an exciting project for many reasons, but most of all, I believe it says to the community that the services and resources of a federally qualified health center are vital to a diversifying and healthy community,” Dykstra said. “I believe our patients, staff and the greater community can take pride in a building that is welcoming and inviting.”
Published in
Iowa PCA Blog
Tagged under






























.png)